Welcome to the website of Dr. Adriaan Louis van Huyssteen, Consultant Orthopaedic Surgeon. Dr van Huyssteen has a special interest, expert training and experience in adult hip and knee surgery.
The hip joint is commonly known as a ball and socket joint and is formed where the rounded head of the thigh bone joins the pelvis. The joint is surrounded and lined by cartilage, muscles, and tendons. It relies on these tissues for support, stability, and ease of movement.
The hip joint functions as one of the most important joints in the human body. Designed for both mobility and stability, the hip allows the entire lower extremity to move in three planes of motion, while providing an important shock absorption function to the torso and upper body. The hip is a ball and socket joint, uniting the femur (thigh bone) with the pelvis. As a result of this configuration, the leg moves forwards and backwards, side to side, and rotates to the right and left.
BONES
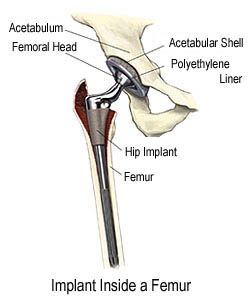
The pelvis features two cup-shaped depressions called the acetabulum, one on either side of the body. The femur, or thigh bone, is the longest bone in the body and connects to the pelvis at the hip joint. The head of the femur, shaped like
a ball, fits tightly into the acetabulum, forming the ball and socket joint of the hip.
CARTILAGE
Embedded within the acetabulum of the pelvis lies an important structure known as articular cartilage. This cartilage has two very important functions. First, the smooth, low friction surface of the cartilage allows the hip joint to move freely in
all planes of movement. Second, the articular cartilage cushions the hip during weight bearing activities, providing an important shock absorption function to the entire lower extremity.
LIGAMENTS
The hip joint also features a complex system of ligaments that provide stability for the pelvis and lower extremity. The ligaments of the hip joint connect the femur to the pelvis and are essential to keeping the hip from moving outside of its
normal planes of movement.
MUSCLES
The muscles of the hip joint have dual responsibilities. They provide the dynamic functions necessary to raise and lower the lower extremity as well as the stabilizing functions required during standing, walking, or other weight-bearing
exercises. This complex system of muscles works synergistically to provide the power for the hip to move in all directions, as well as to stabilize the entire lower extremity during weight bearing activities.
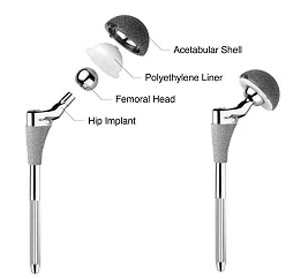

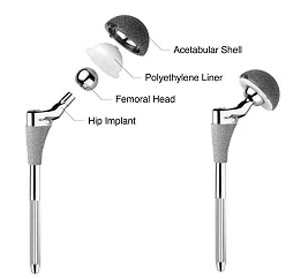
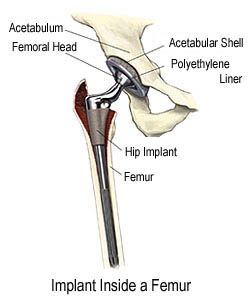
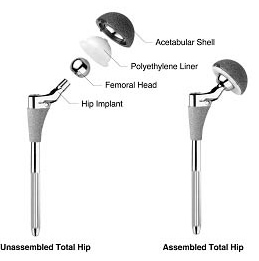
In a total hip replacement surgery, the painful parts of the damaged hip are replaced with artificial hip parts called a prosthesis, a device that substitutes or supplements a joint. The prosthesis consists of steel components: a socket, ball, and stem. The outer shell of the socket is usually made of metal and the inner shell consists of plastic, or the entire socket may be plastic. When the metal ball is joined with the socket, the new hip can allow for smooth, nearly frictionless movement.
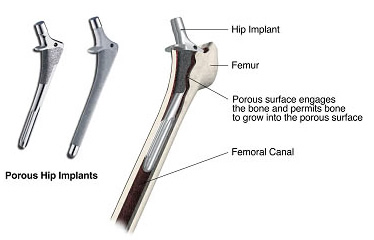
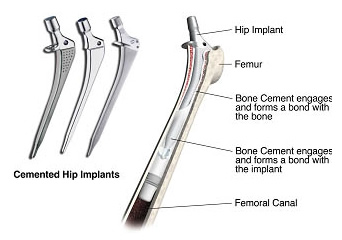
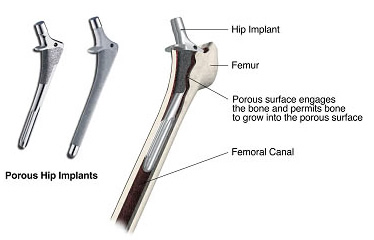
There are two main types of fixation philosophies-cemented and porous. Both can be effective in the replacement of hip joints. The physician (and the patient) will choose the best solution that is specific to the patient's needs.

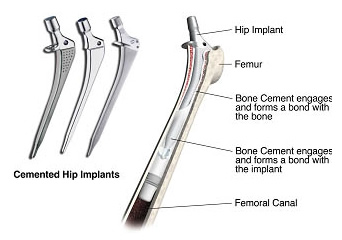
The cemented hip implant is designed to be implanted using bone cement (a grout that helps position the implant within the bone). Bone cement is injected into the prepared femoral canal. The surgeon then positions the implant within the canal and the grout helps to hold it in the desired position

The porous hip implant is designed to be inserted into he prepared femoral canal without the use of bone cement. Initially, the femoral canal is prepared so that the implant fits tightly within it. The porous surfaces on the hip implant are designed to engage the bone within the canal and permit bone to grow into the porous surface. Eventually, this bone ingrowth can provide additional fixation to hold the implant in the desired position.
If you and your surgeon decide that total hip replacement is right for you, a date will be scheduled for your surgery. Several things may be necessary to prepare for surgery. For example, your surgeon might ask you to have a physical examination by your primary care physician. This will help to ensure that other health problems you may have, such as diabetes or high blood pressure, will be identified and treated before surgery.
You doctor may suggest that you lose weight and initiate an exercise programme. If you smoke, be sure to speak with your doctor about it, as smoking can dangerously increase surgical risks and slow down the healing process.
You should also finish any dental work that may be underway to prevent germs in your mouth from entering the bloodstream and infecting the joint. It is likely that you will need blood during hip surgery, and your surgeon may place an order with the blood bank in case a transfusion is needed. If you prefer, or if your surgeon feels it is needed, you may want to donate your own blood ahead of time to reduce the risk of your body reacting to the blood transfusion.
On the day of surgery, an intravenous tube will be inserted into your arm to administer necessary medications and fluids during surgery. You will then be taken to the operating room and given anesthesia.
The surgery usually takes two to four hours, although this is dependent upon the severity of the arthritis in your hip. In the operating room, a urinary catheter will be inserted and left in place for one or two days. Compression stockings and pneumatic sleeves will be put on both legs.
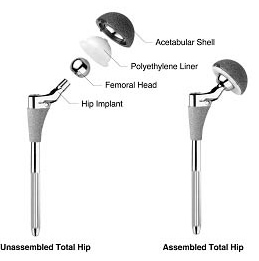
The procedure is performed through an incision over the side of the hip. The ball-end of the thighbone (femur) is cut and replaced with the new metal ball and stem component. It may be stabilized with or without cement. The damaged surface of the socket is smoothed in preparation for the insertion of the new socket. The ball and socket are then joined. When the surgeon is satisfied with the fit and function, the incision will be cleaned and covered with dressings. You will also find small drainage tubes coming out of the hip to drain fluid from the wound.
You will be sent to the recovery room and as the anesthesia wears off you will slowly regain consciousness. A nurse will be with you, and may encourage you to cough or breathe deeply to help clear your lungs. You will also be given pain medication and will find a foam wedge or pillows placed between your legs to help hold your joint in place. When you are fully conscious, you will be taken back to your hospital room.
When you are back in your hospital room you will begin a gentle rehabilitation programme to help strengthen the muscles around your new hip and regain your range of motion. On the day of surgery you may be asked to sit on the edge of the bed and dangle your feet. You will also learn how to protect your new hip while doing daily activities.
As soon as possible, usually within the next 24 hours, your physical therapist will help you start walking a few steps at a time. As you heal you will progress from walker to crutches and then a cane. Before you are dismissed from the hospital, an occupational therapist will also show you how to perform daily tasks at home with your new hip. For example, he or she will instruct you on how to go to the bathroom, how to dress yourself, how to sit or stand, how to pick up objects and many others.
After about two to four days, or when your surgeon determines that you have recovered sufficiently, you will be discharged. You may be transferred to a rehabilitation facility for a few more days, as determined by your surgeon. Upon returning to your home, you will need to continue taking your regular medications and continue exercising as directed by your surgeon or physical therapist. Walking, remaining active and practicing the required exercise are the quickest ways to full recovery.
Longevity of the prosthetic hip varies from patient to patient. It depends on many factors, such as a patient's physical condition, activity level, and weight, as well as the accuracy of implant placement during surgery. It is useful to keep in mind that prosthetic joints are not as strong or durable as a natural, healthy joint, and there is no guarantee that a prosthetic joint will last the rest of a patient's life.
Today, total hip replacement has become a common and predictable procedure. Many patients enjoy relief from pain and improved function, compared to their status before surgery. As a result, some patients may have unrealistic expectations about what the prosthetic hip can do and how much activity it can withstand. As with any mechanical joint, the ball and socket components move against each other. Natural fluid in the joint space, called synovial fluid, helps to lubricate the implants just as it lubricates the bones and cartilage in a natural joint. Still, the prosthetic components do wear as they roll and slide against each other during movement. As with car tires or brake pads, the rate of wear depends partly on how the hip joint is used. Activities that place a lot of stress on the joint implants, as may be the case with heavier and more active patients, may reduce the service life of the prosthesis. Implant loosening and wear on the plastic portions of the implant can lead to the necessity for revision surgery to replace the worn components, or all of the components. Your doctor will be in the best position to discuss these issues with you, taking into account your particular clinical circumstances, the type of implants used, and your post-surgical lifestyle.
Talk with your doctor about the following points, and how they might affect the longevity and success of your hip replacement:
- Avoiding repetitive heavy lifting
- Avoiding excessive stair climbing
- Maintaining appropriate weight
- Staying healthy and active
- Avoiding "impact loading" sports such as jogging, downhill skiing and high impact aerobics
- Consulting your surgeon before beginning any new sport or activity
- Avoiding any physical activities involving quick stop-start motion, twisting or impact stresses
- Avoiding excessive bending when weight bearing, like climbing steep stairs
- Not lifting or pushing heavy objects
- Avoiding low seating surfaces and chairs.
|